ATLANTA — When I was diagnosed with polycystic ovary syndrome last year, relief came first.
Don't get me wrong, the other feelings would follow in short order. Fear of the unknown, anxiety about the future, and the heavy sadness that comes with medical confirmation that "something is wrong."
Still, relief came first. Something was wrong, but I finally knew what it was.
My PCOS diagnosis didn't come easily. During my annual exam a year prior, my OBGYN asked how long I'd been taking the birth control pill. I told her the truth, that it was prescribed to me at 15 years old to mitigate painful menstrual cramps.
"And you've been on it ever since?" she asked. I detected an undercurrent of surprise in her voice, which made me feel a little defensive and embarrassed. I just shrugged and nodded. I honestly had never thought twice about it.
"If you're thinking of starting a family in the next couple years, you might want to come off it," she told me. "See what your cycle does naturally."
Savannah Levins is hosting a live Q&A with PCOS experts. You can watch the livestream on my Facebook page at 7 p.m. on Wednesday, Sept. 4.


In my career as a journalist, I never thought I'd publish an article about my period. But here we are; it never came.
After about five months, I called my doctor to tell her my cycle still hadn't regulated.
"It can take a while since you've been on the pill so long," she told me. "Don't worry yet."
But I was worried, particularly when other symptoms began to manifest. I quickly gained 25 pounds that I couldn't seem to shake no matter what I did. I was eating healthy balanced meals and going to the gym multiple days a week (more so than usual if we're honest, as my wedding was quickly approaching).
I asked my primary care doctor about it, but he brushed it off, saying that gaining weight "just comes with age." He said I wasn't obese, so he wasn't worried. But I was still convinced it didn't seem right. So I sought out the opinion of another doctor, who told me the same. Then, a third who told me eating less carbs might help. That'll be another $250 copay, please.
After about 8 months, an officially overweight BMI, and still no period -- I went to a new OBGYN to plead my case.
"I know my body," I said. "And I'm telling you, something is wrong."
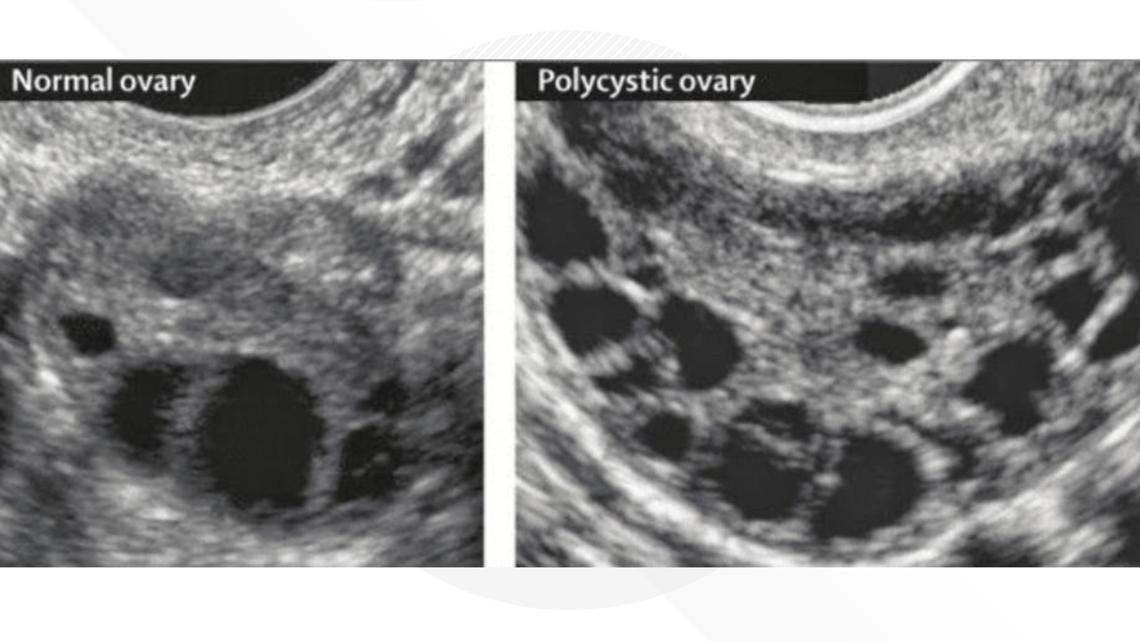
So she agreed to do an ultrasound of my uterus. As I lay on the table, sweaty fists clenched with nerves, I saw the image pop up on the computer screen. I didn't know what exactly what I should be seeing (I majored in journalism, not medicine, after all). But I felt in my gut that something didn't look right.
Why were there so many...holes? Why was the initially bubbly and chatty sonographer suddenly quiet? Why was she counting those little holes (follicles, I'd learn later)? Why were there so many of them? I realized each time she clicked the computer mouse, she was counting another. I started counting along in my head. Click. 41. Click. 42. Click, click, click.
Savannah Levins is hosting a live Q&A with PCOS experts. You can watch the livestream on my Facebook page at 7 p.m. on Wednesday, Sept. 4.

"Is it supposed to look like that?" I finally blurt out.
Of course, she couldn't tell me anything aside from "the doctor will go over it with you." Then she ushered me into another room for bloodwork.
Not long after, though it felt like an eternity, my doctor settled into the chair across from me and laid it all out. "We still have to wait on the blood results," she said. "But you meet the criteria for PCOS."
Remember that relief I talked about? It was mixed with a bit of indignant gratification, too.
"I knew I wasn't crazy," were the first words out of my mouth. After nearly a year of fighting for an answer, I finally had one. My next words, the ones I would have expected to come first, were: "what is PCOS?"
She explained that PCOS is a hormonal imbalance that occurs when someone's ovaries create excess hormones. Those androgens can cause your reproductive hormones to become imbalanced, resulting in a bevy of super fun symptoms like weight gain that's particularly difficult to lose, insulin resistance, acne, irregular periods, abnormal hair growth on the body, thinning hair on the head, skin tags, mood swings, and infertility.
Hearing that last one was what brought my relief crashing down into tearful fear.
My journalism degree turned out to be useful in this doctor's office, after all. I had a thousand questions poised and ready to go.
Questions after a PCOS diagnosis
What caused this?
Experts don't know. Some studies indicate it could be genetic, though no one in my family had ever been diagnosed with, or even heard of, PCOS. Other studies suggest nutrition could play a role. Other researchers have posed the hypothesis that obesity and insulin resistance could be a cause, although it's really a 'chicken or the egg' situation. The link there is clear, but it's hard to tell which might be a symptom of the other.
Can I reverse it?
No. Some symptoms can be managed with medication and lifestyle changes, but there is no cure.
Is this uncommon?
Also no.
The World Health Organization estimates that 8–13% of women of reproductive age have PCOS. Other groups have estimated that number to be closer to 20%. Some women may have PCOS and never know it, because they don't have any outwardly obvious physical symptoms. My bloodwork, tests not normally ordered by primary care doctors or OBGYNs, confirmed things my past medical providers never suspected, including abnormally high levels of testosterone and Anti-Müllerian Hormone (AMH).
In the 15 months since my diagnosis, I've been working to manage my PCOS with a lot of trial and error. It's involved a lot of medications: ones that force a mensural cycle, others that initiate ovulation, others that help control insulin levels with the added benefit of weight loss.
I was also told my five days a week doing cardio at the gym was probably doing more harm than good, since cortisol (stress) levels are higher in women with PCOS. So I switched to lower impact workouts like Pilates and barre, and tried to mitigate my insulin resistance with a Mediterranean based diet.
I've bought more books, joined more Facebook groups, followed more podcasts, and read more articles about PCOS than I can count. I wanted to know everything I could about PCOS and let me tell you, there's a lot out there.
To that end, this is the part of my story where I'm wavering on how to proceed. I'm hesitant to delve into what's worked for me, and what hasn't, and how it's affected my life symptomatically. Because as it relates to PCOS, the one thing I know for a fact is that everyone is different.
Some people with PCOS are able to get pregnant no problem, others have spent years desperately working with fertility specialists to no avail. Some gain extra weight and can't lose it on their own, others never gain a single unwanted pound. Some have facial hair they have to grapple with their whole lives, others don't. Some have painful cysts on their ovaries, others don't.
So here I am, a journalist with a million questions, and honestly very few definitive answers to offer you. What I can do, though, is share my story and use my platform to help raise awareness.
September is PCOS Awareness Month. The first time it rolled around, I was honestly too overwhelmed to acknowledge it. Very few people even knew about my diagnosis at that time. Although today I'm still looking for answers, I feel more prepared to seek and share them publicly.
Savannah Levins is hosting a live Q&A with PCOS experts. You can watch the livestream on my Facebook page at 7 p.m. on Wednesday, Sept. 4.


I recently reached out to a few PCOS experts I've followed over the last year and asked if they'd be willing to participate in a live Q&A. They all, immediately, said yes. I was humbled and appreciative but not surprised. The PCOS community, often affectionately referred to as a "cysterhood," is an incredibly supportive one.
At 7 p.m. on Wednesday, Sept. 4, we will host the live Q&A on Facebook.
If you have, or suspect you have, PCOS, it will be a great opportunity to ask questions of these these leading experts we might not otherwise have access to. Even if you don't have PCOS, I invite you to tune in. Because statistically, someone you know or love is living with this condition.
Knowledge can be scary and overwhelming but it is -- as the saying goes -- power.
You can watch the livestream on my Facebook page. It will also be shared on the 11Alive News Facebook page and later uploaded to 11Alive's YouTube Page.
PCOS Q&A panelists
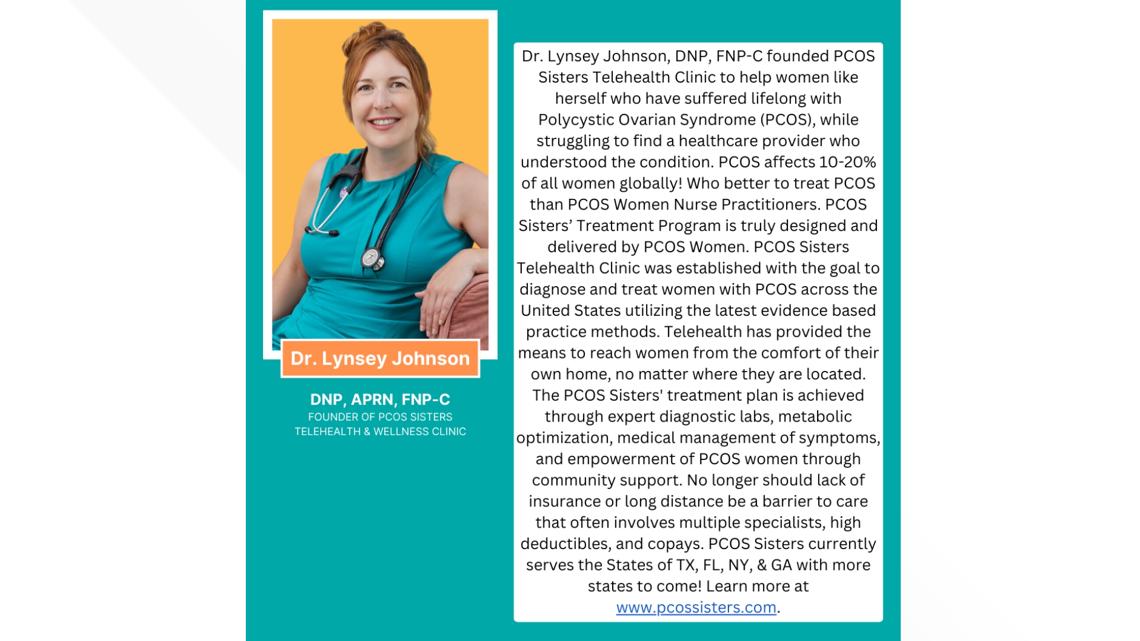
Dr. Lynsey Johnson, founder of PCOS Sisters telehealth clinic

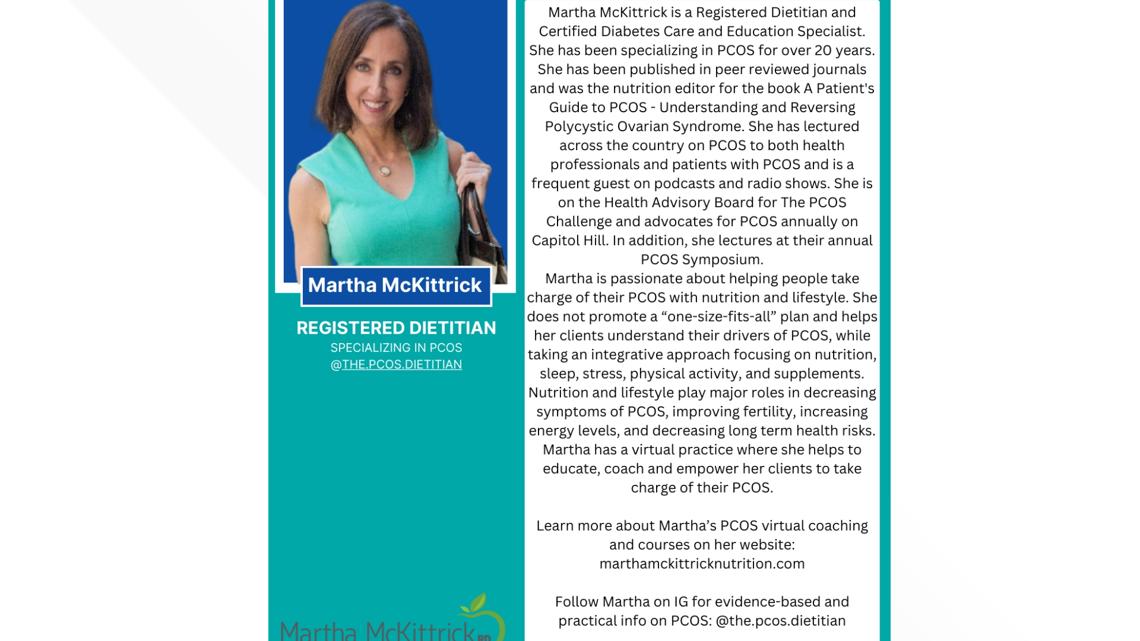
Martha McKittrick, a dietitian specializing in PCOS

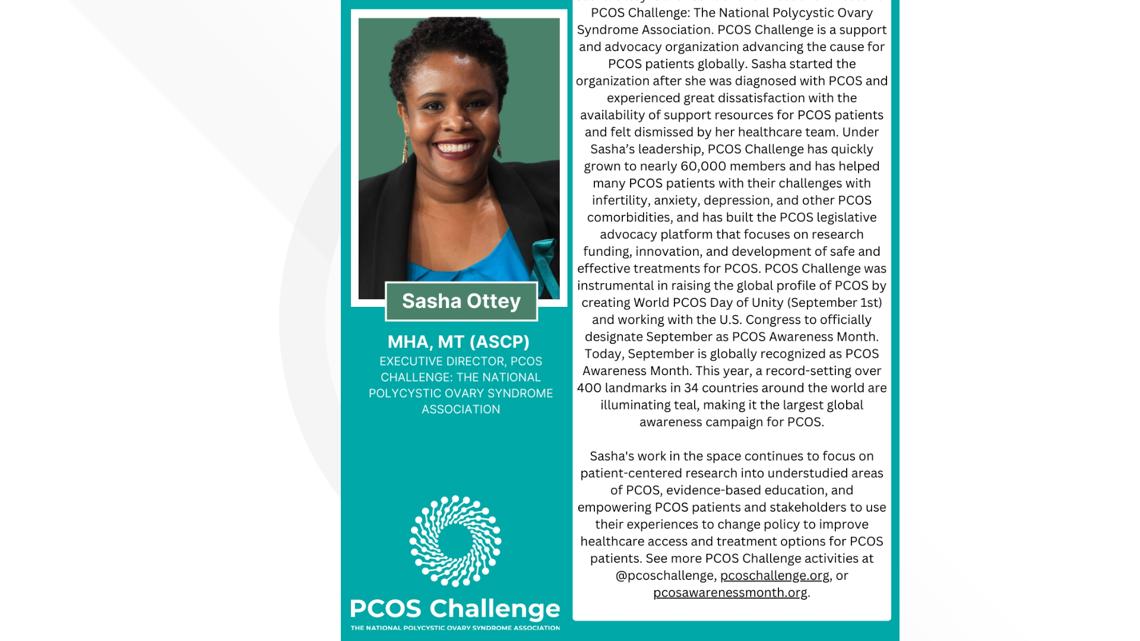
Sasha Ottey, Executive Director at PCOS Challenge: The National Polycystic Ovary Syndrome Association