ATLANTA — Hundreds of people want money for lost wages and unpaid medical bills after allegedly being injured by a COVID-19 related treatment.
The federal government has a little-known program called the Countermeasures Injury Compensation Program (CICP) that says it can help. But, so far, it has approved only a handful of claims.
11Alive's investigative team, The Reveal, has been trying for nine months to learn more about the program and the claims denied. This week, we finally received some answers.
The information is still very limited due to privacy laws around medical information. CICP started taking claims in 2010 when the government wanted people to get the H1N1 vaccine. About 400 people filed claims back then, believing they had somehow been injured by the shot. Then, the program got quiet with just a handful of claims for treatments associated with smallpox and anthrax.
Then came COVID-19. The Reveal has learned 641 claims – more than any other countermeasure – have been filed so far across the country. To be fair, more than three times as many COVID-19 vaccine shots have been given than H1N1 and we don’t have three times as many claims. To some, it’s proof treatments for COVID-19 are safe.

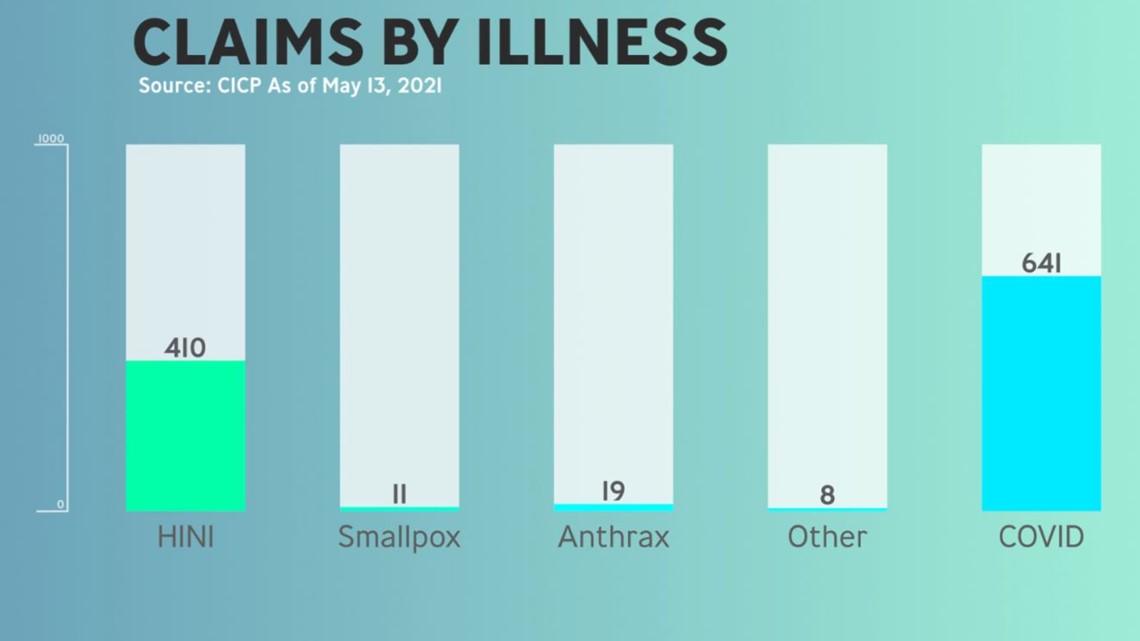
Others feel the data shows that even when a treatment is deemed safe, it is not without some risk. The CICP warns that filing a claim doesn’t mean the injury is actually related. At least in the CICP’s eyes, it's generally not.
Before COVID-19, the CICP denied 92% of the claims. Information obtained through our Freedom of Information Act request indicates most of those denials were because the person didn’t provide the necessary documentation or couldn’t prove their injury was related.
The CICP said it hasn’t made any decision about the COVID-related cases. Those injuries range from an allergic reaction to paralysis, but the most common is death.
About 100 of the claims related to death seem to have more to do with what the government didn’t do. The context of the claims appears connected to nursing home care and a lack of training on infection control.
“Failure to have infection control programs in place, the failure to have adequate infection control in place, the failure to properly train staff, the failure to provide sufficient staff, the failure to cohort infected and uninfected individuals, the failure to provide PPE to staff and residents, the failure to train on the proper use of PPE, the failure to have adequate procedures in place to deal with infection, the failure to adequately monitor residents for signs of infection, the failure to transfer residents to a higher level of care when needed, the failure to adequately treat residents with COVID, the failure to provide appropriate distancing among residents, the failure to properly report the number of COVID-19 cases and deaths to authorities, and others," according to a CICP report.
About twice as many claims, 182, have something to do with the use of a ventilator. Thirteen are associated with the vaccine, and 81 applications don’t say what treatment they think caused their loved one to die.
The CICP is considered the payer of last resort. If a claim is approved, the CICP will only reimburse lost wages and unpaid medical bills, so some of the people claiming injuries might be approved, but receive no compensation because they didn’t stop working and health insurance paid for their doctor’s visits.
You only have one year from the date of your injury to file and The Reveal did find claims denied because applicants missed the deadline. Here’s a link to learn more: https://www.hrsa.gov/cicp
The Reveal is an investigative show exposing inequality, injustice, and ineptitude created by people in power throughout Georgia and across the country.